Free excerpt from Assessment and Treatment of Muscle Imbalance: The Janda Approach
 Causes of Muscle Weakness
Causes of Muscle Weakness
Muscle tension can decrease as a result of a structural lesion in the CNS such as a spinal cord injury or stroke. A loss of tension leads to flaccidity or weakness. Weak muscles are also described as hypotonic or inhibited. Functionally, muscle can be weak as a result of neuroflexive or adaptive changes and may exhibit delayed activation in movement patterns.
Neuroflexive Factors for Decreased Tension
Many contractile factors can contribute to decreased muscle tension:
- Reciprocal inhibition (Sherrington 1907). Muscle becomes inhibited reflexively when its antagonist is activated. Weakness is often reflex-mediated inhibition secondary to increased tension of the antagonist.
- Arthrogenic weakness (Stokes and Young 1984; DeAndrade, Grant, and Dison. 1965). Muscle becomes inhibited via anterior horn cells due to joint swelling or dysfunction. This weakness also leads to selective atrophy of Type II fibers (Edstrom 1970).
- Deafferentation (Freeman, Dean, and Hanham 1965). Deafferentation is a decrease in afferent information from neuromuscular receptors. Damage to joint mechanoreceptors (as seen with ligamentous injury) with subsequent loss of articular reflexes can cause altered motor programs, often influencing many muscles remote from the injured area (Bullock-Saxton 1994). This loss of afferent information ultimately leads to de-efferentation, or the loss of efferent signals to alpha motor neurons, which results in decreased muscle strength.
- Pseudoparesis (Janda 1986a). Pseudoparesis is a clinical presentation of weakness of neuroflexive origin. Pseudoparesis has three clinical signs: hypotonia upon inspection and palpation, a score of 4 out of 5 on a manual muscle test, and a change in the muscle activation pattern that may include delayed onset with early synergist activation or decreased EMG levels. Facilitatory techniques often restore muscle strength and activation. Normally facilitatory input can be inhibitory to a pseudoparetic muscle (Janda 1986a).
- TrP weakness (Simons, Travell, and Simons 1999). Hyperirritable bands of muscle fiber decrease the stimulation threshold, leading to overuse, early fatigue, and ultimately weakness. Muscles with active TrPs fatigue more rapidly than normal muscles do (Mense and Simons 2001), and they exhibit a decreased number of firing motor units and poor synchronization (Janda 1993).
- Fatigue. Muscle fatigue can be caused by metabolic or neurological factors. Often during exercise muscles are fatigued before pain is experienced. Thus the patient develops compensatory and faulty movement patterns before experiencing pain.
Adaptive Factors for Decreased Tension
Noncontractile factors causing decreased muscle tension are stretch weakness and tightness weakness:
- Stretch weakness (Kendall, McCreary, and Provance 1993; Sahrmann 2002a, 2002b). Stretch weakness is a condition in which a muscle is elongated beyond physiological neutral but not beyond the normal ROM (Janda 1993). Prolonged muscle elongation causes muscle spindle inhibition and the creation of additional sarcomeres. The increased muscle length also changes the length–tension curve. Stretch weakness is also known as positional weakness and is often associated with overuse and postural changes.
- Tightness weakness (Janda 1993). This is the most severe form of muscle tightness. It is often overlooked clinically. Overused muscle shortens over time, changing the muscle’s length–tension curve and becoming more readily activated and weaker after time. There is also an increase in the noncontractile tissue and a decrease in elasticity, leading to hypertrophy. Ultimately, overuse leads to ischemia and degeneration of muscle fibers, which further weakens the muscle.
When an inhibited and weak muscle is resisted, as is the aim of strengthening exercises, its activity tends to decrease rather than increase (Janda 1987). It is important to distinguish between neuroflexive weakness and structural weakness. Often, if the tight antagonist is stretched, the weak and inhibited muscle spontaneously increases in strength.
Janda’s Classification of Muscle Imbalance Patterns
Through his observations of patients with neurological disorders and chronic musculoskeletal pain, Janda found that the typical muscle response to joint dysfunction is similar to the muscle patterns found in upper motor neuron lesions, concluding that muscle imbalances are controlled by the CNS (Janda 1987). Janda believed that muscle tightness or spasticity is predominant. Often, weakness from muscle imbalance results from reciprocal inhibition of the tight antagonist. The degree of tightness and weakness varies between individuals, but the pattern rarely does. These patterns lead to postural changes and joint dysfunction and degeneration.
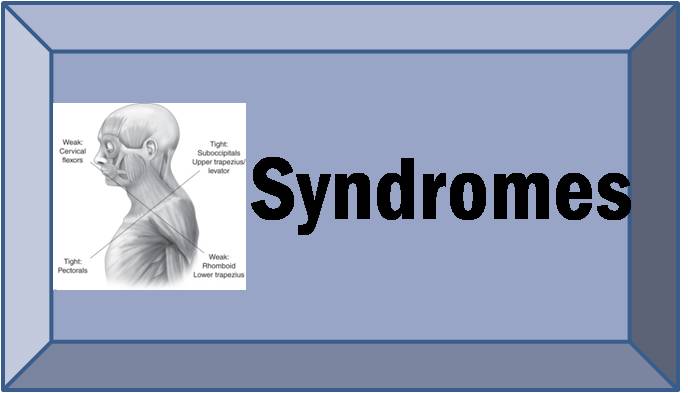
Janda identified three stereotypical patterns associated with distinct chronic pain syndromes: the upper-crossed, lower-crossed, and layer syndromes. These syndromes are characterized by specific patterns of muscle weakness and tightness that cross between the dorsal and the ventral sides of the body.